Reckoning with the relation between stressors and suicide attempts in a time of Covid-19
Reckoning with the relation between stressors and suicide attempts in a time of Covid-19
Abstract
The Covid-19 pandemic presents a unique set of risk exposures to populations, which may lead
to an increase in suicide. While large-scale traumatic events are known to increase psychological
disorders, thus far the science has not shown a clear link between these events and suicide. In
their paper in this issue, Elbogen and colleagues (Am J Epidemiol. 2020;(XX):XXXX–XXXX)
use representative data from the National Epidemiologic Survey on Alcohol and Related
Conditions (NESARC) to show that four dimensions of financial strain—financial debt/crisis,
unemployment, past homelessness, lower income—are associated with subsequent suicide
attempts. There are three main learnings we may take from Elbogen et al: first, with populations
facing record-breaking unemployment, economic recession, and reduced wages, we can
anticipate an increase in suicide in the wake of the Covid-19 pandemic. Second, these data show
the centrality of financial stressors, marking the current moment as distinct from other disasters
or large-scale trauma. Third, the data teach us that financial stressors are linked, and cumulative.
In this way, the paper is a sobering harbinger of the potential effects on suicide of the collective
stressors borne by the Covid-19 pandemic and other mass traumatic events that are accompanied
by substantial financial stressors.
Key words: financial stressors, mental health, economic recession, suicide, trauma,
unemployment
Reckoning with the relation between stressors and suicide attempts in a time of Covid-19
In their paper in this issue of the American Journal of Epidemiology, Elbogen and colleagues (1)
(Am J Epidemiol. 2020;(XX):XXXX–XXXX) use representative data from the long-standing
National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), to show that
four dimensions of financial strain—financial debt/crisis, unemployment, past homelessness,
lower income—are associated with subsequent suicide attempts. They show that the influence of
these four financial stressors was cumulative. Importantly they show that reporting all four of
these stressors was associated with a twenty-fold increase in predicted probability of suicide
attempts. This paper adds to a growing literature that has shown both that suicides increase in
populations exposed to financial stressors (2–4), and that financial stressors are associated with a
range of adverse health indicators (5–7). It brings however a robust approach showing this
association longitudinally in a population-based survey, giving us further confidence that
financial stressors are indeed associated with greater risk not only of morbidity, but also
mortality, in the relatively short term.
This paper also brings some clarity to the literature about the relation among large-scale
traumatic events (e.g., natural disasters) and suicide. Although large-scale traumatic events have
been amply shown to lead to an increase in a broad range of psychiatric disorders (8), including
mood-anxiety disorders that are themselves associated with increased risk of suicides (9), the
science thus far has not shown that large-scale traumatic events are associated with risk of
suicide itself (10). The Elbogen paper (1) suggests that this may be due to the central role that
financial stressors may play in the occurrence of suicide. The vast majority of large-scale
traumatic events are, luckily, simply not consequential enough to cause deep and wide
population-based financial effects, and it may well be that it is the absence of this effect that
explains why there is no apparent link between disasters and subsequent suicide risk. That would
reconcile the disaster literature with the literature on economic recessions that has indeed shown
a link between broad economic function and risk of suicide. (3,11,12)
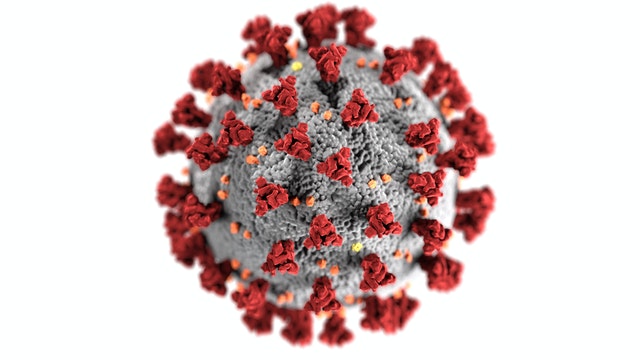
To read and understand Elbogen’s and colleagues’ work in 2020 without seeing it through the
lens of the current Covid-19 moment would be a challenge. The first six months of 2020 were
marked by the advent of the novel SARS-CoV-2 pathogen, hundreds of thousands of unexpected
deaths worldwide, and efforts to mitigate the risk of the virus that occasioned an unprecedented
economic collapse that mirrored in depth and scope the great recession of the 1930s. In the US,
36 million people filed for unemployment in several months as businesses shut down and
economic opportunity evaporated. This economic effect was not evenly distributed. Persons who
were already employed in low-income jobs were more likely to be unemployed, as were persons
of color who had fewer savings and less wealth to begin with, which is associated with increased
mental illness. (13) As a direct result, in a short period of time the US, and many other countries
worldwide, went from the longest period of economic expansion in a century, to a wide-spread
economic shock triggering broad-based financial stressors that affected those who were most
economically vulnerable the most.
What therefore does the Elbogen paper (1) portend for the current moment? Unfortunately, these
data do not bode well for what we may see in the near future. If these data hold, we may expect
to see a rise in suicide attempts, and presumably death from suicide, in the coming months and years, particularly among persons who are economically vulnerable and already marginalized.
Early data showing a dramatic increase in mood-anxiety disorders during the Covid-19 pandemic
(14) further supports this projection. If Elbogen and colleagues (1) are right, and there is every
reason to think that they are, we will witness an increase in suicide that will add to the excess
mortality that we can expect in the aftermath of Covid-19, adding, sadly, to the anticipated deep
and lasting health consequences of the pandemic and its long-tail economic shadow.
How should we then, as epidemiologists, think of the moment, informed by the Elbogen paper
(1)? Can we use what we are learning here to inform efforts to mitigate the expected increase in
suicide, nudging us to pragmatic solutions that can help create a healthier population? There is
much to admire about the Elbogen paper (1), in both its design, data used, and execution. This
gives us confidence that we can, from this work, learn. We suggest that there are three
observations that emerge from this paper that can point to solutions in the moment.
First, simply the awareness of an anticipated increase in suicide should inform our messaging,
and shape the vocabulary that informs the public health conversation. Behavioral health is
responsive to social and economic circumstance—as shown here—but also to culture and the
broader public conversation. We know that raising awareness off and calling attention to risk of
suicide in specific populations can mitigate its risk (15). It seems rational that a similar approach
in this particular moment can have a similarly protective effect. As with all predictions, here
informed by the Elbogen data (1), we would expect an increase in suicide in the post-Covid-19 ORIGINAL
moment only if we do not do anything different to change underlying conditions. One of the easiest elements of those conditions to change would be public awareness of, and education
about suicide, making concerted efforts to elevate visibility of this issue urgent in the moment.
Second, these data show the centrality of financial stressors to the risk of suicide, and, as noted
earlier, distinguish the risks in the current moment as distinct from the risks present after
disasters. This points to potential solutions. There is abundant reason for providing financial
support to populations who need it in the aftermath of this pandemic as an instrumental path to
recovery of social function that in and of itself is associated with health. However, recognizing
that relief of financial stressors can be an intervention that reduces the risk of suicide could,
perhaps, provide a further compelling argument for such an approach in the Covid-19 moment.
Arguments for and against economic supports that alleviate financial stressors in the current
Covid-19 moment have tended to be shaped by ideological and partisan divides, resting on belief
systems that are not grounded in what the moment may call for. Can recognizing that mortality—
specifically suicide—is a risk that we incur absent alleviating financial stressors, help inform and
inflect the national conversation towards innovative efforts to alleviate financial strain during
this time?
Third, these data teach us that financial stressors are linked, that their effect is cumulative. This
may suggest that prevention strategies floated in the public conversation to alleviate financial
strain, focusing on only one dimension of stressor, may simply be insufficient to mitigate the
effect of financial strain on suicide. (16) For example, income support may have a positive effect
on multiple dimensions of living, but it may be insufficient when one recognizes the tangled
effects of housing, income, employment, and that these forces co-occur, defying our reductive efforts at simple counterfactuals that isolate the effect of any single one of these influences.
Support for housing, as another example, may also be limited in and of itself, unless it is
accompanied by efforts to make sure we alleviate the other set of financial stressors that may
persist even if one is housed affordably, particularly in the context of complex national economic
circumstances. This suggests that it is comprehensive efforts to alleviate stressors, to replace lost
or missing assets—at the financial, relational, and community level—that ultimately are needed
to protect populations from increased suicide risk at a time of great national trauma.
Questions remain. This work does not tackle the role of financial stressors in shaping inequities
in suicide, along socioeconomic or racial/ethnic lines that shape so much of our health indicators.
Suicide has long defied simple demographic characterization (17) and this paper is no exception.
Understanding, however, the role of financial stressors in narrowing or widening health gaps
becomes particularly important during a moment when a pandemic, and its economic
consequences, are being experienced unevenly, when underlying gaps both are shaping the
consequences of the pandemic and being shaped by it. This agitates for us to do more work on
the area informed by a health equity lens, prioritizing work that helps us understand how
financial stressors may or may not intersect with these powerful demographic forces, and how
that shapes the complex web of forces that must be mitigated to reduce risk of suicide in
particular groups. Carrying out such work will not be straightforward, and may require data that
extend beyond the scope of the data that currently are available to us. It is plausible that the
Covid-19 era may present us with such data. Now that we understand, thanks to the Elbogen ORIGINAL
paper (1) the centrality of complex financial stressors to the risk of suicide we can turn our attention to understanding how these stressors work together, and as such where we can best
intervene.
The current Covid-19 moment sharpens the mind and can help focus our thinking on the role of,
and purpose, of our work. That is both appropriate and helpful as we aspire to produce an
epidemiology of consequence (18). It is worth reflecting that the Elbogen paper (1) was clearly
conceived and written well before any of us had ever imagined Covid-19 and its consequences. It
was, however, work that was informed by what we knew, and grounded in an effort to better
understand an important problem. That was, in and of itself, sufficient to create work that has
real valence at the right moment, and that moment happens to be now. Suicide however has long
been an intractable cause of mortality. It stands alone among the major causes of death that has
hardly budged over the past century, even as our rates of mortality from other major causes has
dropped, often dramatically, during that same time period (19). This makes suicide an important
area of inquiry, and understanding the determinants of suicide, the drivers that might be
manipulability and create room for intervention, presents a clear opportunity for scholarship that
leads to action. Elbogen and colleagues (1) do just that with this paper. Even as we have learned
much, and have much to learn still, we now have data that can guide action that can improve
health in the short term. It shall fall to future work to elaborate on this study and show us how
interventions may best be designed, informed by this study, that, within the complex web of
stressors that drive suicide, make the biggest strides towards improving population health.






Comments
Post a Comment